How Autophagy Through Fasting Improves Insulin Sensitivity
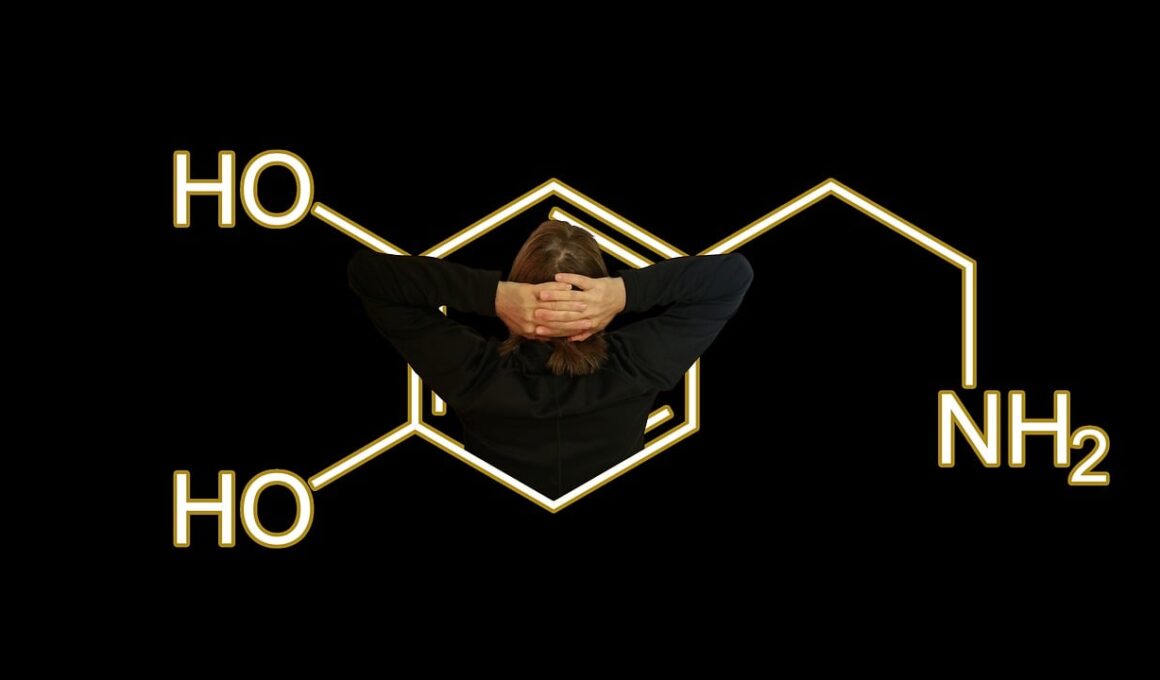
Fasting has gained recognition as a powerful health tool, particularly regarding autophagy and its role in enhancing insulin sensitivity. Autophagy is a vital cellular process wherein cells degrade and recycle dysfunctional components, helping maintain cellular health and function. During periods of fasting, the body shifts its focus from digestion to repair and regeneration. This process can lead to improved glucose metabolism, reduced insulin resistance, and enhanced insulin sensitivity. Insulin sensitivity is crucial as it determines how effectively the body can utilize insulin to regulate blood sugar levels. As one practices fasting regularly, cellular stress responses activate pathways that trigger autophagy, promoting metabolic health. Studies suggest that autophagy can aid in protecting against type 2 diabetes, reducing systemic inflammation, and improving overall metabolic flexibility. Fasting not only stimulates autophagy but also contributes to the production of beneficial hormones that further enhance insulin sensitivity, thereby potentially reducing the risks associated with metabolic disorders. Understanding the relationship between fasting and autophagy opens avenues for functional health improvements, encouraging more individuals to adopt fasting as a lifestyle choice for better metabolic outcomes.
Fasting methods vary, and understanding these variations can help individuals maximize the benefits they derive from fasting. Different fasting approaches include intermittent fasting, prolonged fasting, and alternate-day fasting. Intermittent fasting, often popular among health enthusiasts, involves cycling between periods of eating and fasting, which can vary from 16 hours of fasting followed by an 8-hour eating window. Prolonged fasting may last 24 hours or longer, focusing on extended periods without food to maximize autophagy benefits. Alternate-day fasting entails alternating between feast and fast days. Each method encourages autophagy to some degree, enhancing insulin sensitivity and supporting weight management. During the fasting period, insulin levels drop significantly, enabling the body to clear excess glucose from the bloodstream, stimulating fat cell mobilization, and promoting weight loss. As insulin sensitivity improves, your overall ability to process carbohydrates enhances, making it easier to manage weight and reduce inflammation. Therefore, selecting a fasting method suited to individual lifestyle preferences can facilitate long-term adherence, creating sustainable habits conducive to metabolic health, especially for those at risk of insulin resistance and type 2 diabetes.
Incorporating food choices during feeding windows can play a crucial role in enhancing the benefits of fasting. Opting for whole, unprocessed foods over refined options can support metabolic health. Foods rich in healthy fats, fiber, and antioxidants, such as avocados, nuts, seeds, leafy greens, and berries, provide essential nutrients while minimizing spikes in insulin levels. Managing carbohydrate intake, particularly refined sugars and high glycemic-index foods, is essential during eating periods to prevent insulin resistance. Pairing carbohydrates with proteins or healthy fats can also promote more balanced blood sugar responses. Fasting periods might be complemented with hydration strategies that focus on water and herbal teas. This supports both cellular function during autophagy and helps manage hunger levels. Nutrition is especially vital right after breaking a fast, as the body requires proper nutrients to recover and restore optimal function. Incorporating nutrient-dense foods can maximize the cellular recovery process initiated by autophagy while reinforcing insulin sensitivity. Ultimately, adopting mindful eating habits during feeding times can significantly improve the fasting experience and outcomes, including enhanced insulin sensitivity and overall well-being.
Research continually illustrates the impact of autophagy on insulin sensitivity, emphasizing how lifestyle changes can mitigate risks associated with metabolic disorders. Enhanced autophagy due to fasting leads to the improvement of various mechanistic pathways that facilitate insulin action. For instance, autophagy regulates the insulin signaling cascade while promoting the degradation of insulin receptor substrates, ensuring a more efficiently functioning system. Additionally, autophagy helps reduce endoplasmic reticulum (ER) stress, which is linked to insulin resistance. Through fasting, the reduction occur in stress levels, thereby optimizing cellular function. The end result is better blood glucose management and improved responses to insulin. Numerous scientific studies have clearly demonstrated the favorable effects of fasting-induced autophagy on the overall body mechanisms responsible for regulating insulin sensitivity. This underscores the growing interest in using fasting as a therapeutic option not just for weight management but also for treating or preventing diseases connected to insulin resistance. With continued exploration, these findings validate the essential connections between fasting, autophagy, and insulin sensitivity, heightening awareness and promoting informed lifestyle choices among individuals seeking better health.
Personal experiences often highlight the psychological and physiological benefits of fasting related to autophagy and insulin sensitivity. Many individuals report improved mental clarity during fasting periods, attributing this enhancement to hormonal balance and the reduction of inflammation. This cognitive boost emerges from the body’s heightened state of alertness during fasting. Studies show that autophagy plays a role in neuronal health, potentially mitigating neurodegenerative diseases, and fostering improved brain function. Alongside these cognitive benefits, the tangible physical transformation often encourages individuals to embrace fasting as a lifestyle. Regular fasting can lead to significant weight loss, enhanced energy levels, and a sense of well-being that fosters sustained motivation for maintaining overall health goals. Furthermore, the social aspect of fasting; shared experiences or community discussions can enhance commitment. Focusing on personal success stories during fasting journeys can create positive reinforcement, contributing to an overall sense of empowerment. Achieving goals related to insulin sensitivity and metabolic health further fuels the determination to pursue healthy habits while promoting an ecosystem of support within a community of like-minded individuals. This underscores the notion of balanced health through fasting.
Conclusion: Embracing Fasting for Health Benefits
Embracing fasting as a health strategy is a transformative journey, harnessing the power of autophagy to improve insulin sensitivity. Continuous shifts in dietary patterns, food choices, and lifestyle habits facilitate positive health outcomes. By understanding the science of fasting and its physiological processes, individuals can make empowered decisions conducive to health and well-being. Autophagy, stimulated by fasting, not only rejuvenates cell functions but also holds significant implications for metabolic conditions. The evidence supporting its efficacy continues to expand. Diverse fasting methods enable customization to fit individual lifestyles while optimizing health benefits. A carefully integrated approach to nutrition before and after fasting periods can enhance results considerably, maximizing autophagy effects and promoting insulin sensitivity. Individuals should maintain consistency, continually monitor their progress, and adjust their approaches as required to sustain motivation and achieve desired health improvements. Being part of a community that supports the fasting lifestyle creates additional motivation for commitment, ensuring continuity in healthy habits. Ultimately, the dynamic benefits of fasting and autophagy can elevate overall health while significantly mitigating risks associated with metabolic diseases, creating lasting change for those who embark on this journey.
As scientific research advances, the future of fasting and its relationship with autophagy and insulin sensitivity promises exciting opportunities. Ongoing studies aim to explore the nuances of these relationships further, revealing more targeted approaches to nutrition, fasting regimens, and health improvement practices. Future investigations may delve into individualized fasting protocols that consider genetics, existing health conditions, and personal lifestyle preferences. This tailored approach could lead to greater efficacy in achieving desired health outcomes. Moreover, public awareness and education on the benefits of fasting can encourage broader acceptance, ultimately leading to healthier societies. Technologies such as applications and tools aimed at tracking fasting patterns and metabolic responses will promote adherence, guiding users through effective fasting practices and lifestyle changes. As fasting continues to gain popularity, understanding the underlying mechanisms of autophagy will remain crucial in framing recommendations and best practices. Integrating nutritional education with fasting methodologies could empower more individuals to harness the benefits of these practices, thereby improving insulin sensitivity and overall metabolic health. The journey towards health can be enriching, promising tremendous improvements through mindful fasting practices and dedicated lifestyles that prioritize well-being.
In summary, the complex interaction between fasting, autophagy, and insulin sensitivity encapsulates significant potential for enhancing human health. As individuals explore fasting practices, the profound physiological changes occurring within their bodies can lead to transformative insights and experiences. This journey involves commitment, patience, and an open mind focused on the technology of nourishing the body while allowing it to heal and regenerate itself. Adaptation to fasting may require time, learning to navigate hunger signals and physiological responses can be a valuable experience, allowing for deeper introspection and self-awareness. Tracking progress and celebrating small victories fosters a positive mindset towards health goals. Integrating community and social interactions cultivates motivation and accountability, creating a collective energy that inspires participants. The pursuit of better insulin sensitivity through fasting helps individuals improve not just physical health but also mental and emotional well-being. The benefits of fasting transcend mere metabolic outcomes, embracing a holistic approach to health. Through sustainable practices, fasting can lead to a fulfilling lifestyle that not only emphasizes bodily health but also enhances overall quality of life and happiness over time.