How Diabetes Impacts Hormonal Health
Diabetes, a chronic condition, profoundly affects various bodily functions, including hormonal health. When blood glucose levels remain consistently elevated, it triggers a cascade of hormonal imbalances. Insulin, the hormone produced by the pancreas, regulates blood sugar levels. In diabetes, either insulin production is insufficient or the body’s cells do not respond effectively to it. This disruption can lead to elevated blood sugar levels, creating significant pressure on other hormones. For instance, glucagon, another pancreatic hormone, can become oversecreted, further worsening glucose control. Moreover, persistent hyperglycemia can lead to complications affecting reproductive hormones such as estrogen and testosterone. This hormonal imbalance can increase the risk of conditions such as polycystic ovary syndrome (PCOS) in women, impacting fertility and menstrual cycles. In men, insulin resistance can lead to lower testosterone levels, resulting in diminished libido and energy levels. It is crucial for individuals with diabetes to monitor their hormonal health closely. Regular consultations with healthcare providers can help mitigate these risks, emphasizing a comprehensive approach to managing diabetes and maintaining hormonal balance effectively.
Hormonal health is critical for overall well-being, and diabetes significantly influences various hormonal pathways in the body. One key hormone affected is cortisol, the stress hormone. When blood glucose levels are consistently high, the body experiences stress, leading to elevated cortisol production. Chronic high cortisol levels can result in a range of issues, such as weight gain, insulin resistance, and even increased cravings for sugary and unhealthy foods, perpetuating a vicious cycle. Additionally, high levels of cortisol can disrupt the balance of sex hormones, contributing to irregular menstrual cycles in women and reduced testosterone levels in men. This situation emphasizes the interconnectedness of diabetes and hormonal health. It’s essential to explore lifestyle changes to counteract these effects. Incorporating stress management techniques, such as yoga and mindfulness, can help lower cortisol levels. Regular physical activity and a balanced diet are also vital in managing blood sugar levels and promoting hormonal equilibrium. Moreover, supplements, such as omega-3 fatty acids and vitamins, may support general hormonal health. Overall, a proactive approach can enhance life quality for individuals impacted by diabetes.
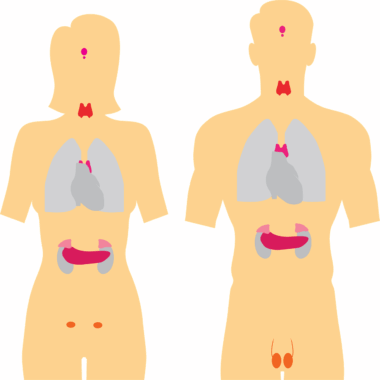
Impact on Thyroid Hormones
The thyroid gland plays a central role in regulating metabolism, energy levels, and temperature, which are critical for maintaining hormonal health. Diabetes can complicate thyroid function, leading to conditions such as hypothyroidism or hyperthyroidism. Individuals with type 1 diabetes are particularly susceptible to autoimmune thyroid disease. The presence of antibodies targeting thyroid tissue can lead to inconsistent levels of thyroid hormones, ultimately affecting metabolic processes. Meanwhile, type 2 diabetes, primarily linked to obesity and insulin resistance, can also associate negatively with thyroid function. This connection may further exacerbate obesity, creating a challenging cycle. Thyroid dysfunction in diabetic patients can present as fatigue, weight fluctuations, and mood changes. Diagnosis of thyroid disorders often occurs through blood tests measuring thyroid-stimulating hormone (TSH) levels, providing insights into the patient’s thyroid status. Effective management requires a holistic strategy, including proper monitoring of both diabetes and thyroid levels. Adjustments in diet, regular screenings, and appropriate medication can be helpful strategies. By ensuring optimal thyroid health, individuals with diabetes can enhance their overall hormonal health and metabolic function.
Insulin’s role in managing diabetes impacts growth hormones significantly, which are essential for tissue growth, repair, and metabolism. In diabetic individuals, inadequate insulin can affect human growth hormone (HGH) production, resulting in various health complications. Typically, human growth hormone and insulin have a synergistic relationship that influences lean muscle mass, fat metabolism, and overall growth rates during development. In children and adolescents with diabetes, disruptions in insulin levels can lead to stunted growth or delayed puberty. Furthermore, adults facing high insulin resistance or prolonged hyperglycemia may experience diminished HGH secretion, affecting muscle repair and recovery. This reduction can be detrimental for those seeking an active lifestyle. Therefore, it becomes vital to prioritize efficient insulin management through balanced meals, regular exercise, and often medication. Strength training may also enhance HGH levels and support metabolic health. Moreover, ensuring adequate sleep can promote HGH secretion. Thus, improving insulin sensitivity can positively impact HGH levels and hormonal health overall, leading to improved energy levels and body composition.
Diabetes and Hormonal Disorders
Diabetes frequently triggers various hormonal disorders, one highly prevalent being polycystic ovary syndrome (PCOS) among women. This condition, characterized by irregular periods, excessive hair growth, and insulin resistance, significantly disrupts hormonal balance. Insulin resistance often exacerbates the symptoms of PCOS, making diabetes a considerable risk factor for its development. Furthermore, this hormonal imbalance can lead to challenges in managing weight and blood sugar levels, creating additional health complications. Moreover, elevated insulin levels associated with diabetes may stimulate the ovaries to produce excess androgens, worsening PCOS symptoms. Men with diabetes aren’t exempt from hormonal disorders either; they may experience low testosterone levels due to insulin resistance and obesity. This decline in testosterone can result in decreased sex drive, mood alterations, and even impacts on metabolic health. As such, understanding the hormonal disorders linked to diabetes is critical for effective management. Regular screenings and collaborative care between endocrinologists and primary care providers can develop personalized treatment plans, include lifestyle modifications, and medications promoting hormonal balance in those dealing with diabetes.
The relationship between diabetes and hormonal health underscores the importance of lifestyle choices in managing both conditions effectively. A nutritious diet can influence insulin sensitivity while also supporting hormonal balance, making it an effective strategy. Incorporating whole grains, lean proteins, and healthy fats can stabilize blood sugar levels while nourishing the endocrine system. Additionally, regular physical activity is crucial for improving insulin sensitivity and managing body weight, which subsequently can have positive effects on hormonal health. Weight management proves essential since both obesity and excess body fat can contribute to insulin resistance and hormonal disturbances. Including cardiovascular exercises and resistance training can aid in blood sugar control. Staying hydrated is another vital practice that can support metabolic processes and hormonal functions. Moreover, sleep hygiene and stress management are also critical for optimal hormonal function. Quality sleep helps regulate hormones, reducing cortisol and enhancing growth hormone levels. Chronic stress management techniques, such as deep breathing or meditation, can help maintain hormonal equilibrium. These holistic approaches can significantly improve an individual’s quality of life for those living with diabetes.
Conclusion
In conclusion, diabetes possesses far-reaching effects on hormonal health, impacting various hormones and contributing to a range of disorders. Strategies focused on improving dietary habits, engaging in regular exercise, and prioritizing stress management can collectively enhance hormonal balance. Monitoring insulin levels, thyroid function, and hormonal profiles remains vital for individuals with diabetes to mitigate risks associated with hormonal dysfunction. Awareness of the interconnectivity among various hormonal systems empowers individuals to take charge of their health and advocate for comprehensive care with healthcare providers. Personalized treatment plans developed collaboratively with healthcare professionals can help individuals navigate the complexities of the condition. Incorporating support networks can further assist in managing diabetes and hormonal health effectively. This journey may include joining support groups or seeking counseling when needed. By understanding the intricate relationship between diabetes and hormonal health, individuals can embark on a path towards improved well-being. The promotion of a healthy lifestyle alongside regular medical supervision can make a significant difference, ultimately leading to better health outcomes for those affected by diabetes and hormonal disorders.
References
For further reading on the connection between diabetes and hormonal health, several resources can provide valuable insights. Books like “Diabetes and Hormonal Health” by Dr. Jane Smith offer an excellent foundation. Websites such as the American Diabetes Association (diabetes.org) provide guidelines on managing diabetes and hormonal health. Consulting peer-reviewed articles can also inform about the latest research findings. Understanding the broad array of resources available aids in developing a more profound knowledge of how diabetes impacts hormonal health and, consequently, overall well-being.