Dietary Strategies for Managing Gastroparesis
Gastroparesis is a chronic condition that affects the stomach muscles, leading to delayed gastric emptying. This disorder can severely impact nutrition and overall health. To manage gastroparesis, dietary changes are essential. A well-structured diet can help ease symptoms and improve quality of life. Patients need to be mindful of food choices, meal timings, and preparation methods. Foods that are easy to digest should be prioritized. Soft, well-cooked meals that minimize digestive effort can be very beneficial. Moreover, smaller, more frequent meals can help to ensure better management of symptoms. Staying hydrated is equally important; fluid intake should be adequate to help digestion. Low-fat and low-fiber foods are generally more suitable. High-fiber options can worsen symptoms by slowing gastric emptying. Foods like bananas, rice, and applesauce often work well in such diets. It’s advisable to keep a food diary to track which foods trigger symptoms. Consulting with a dietitian can provide tailored advice for individual needs, ensuring tranquility in dietary habits while managing this condition.
Understanding the role of nutrition in managing gastroparesis is crucial for stabilizing health. It is advisable to incorporate various food groups into the diet to ensure adequate nutrition. Protein sources such as eggs and fish can help maintain muscle mass without overwhelming the digestive system. Dairy products may be tolerated by some but should be approached carefully. Choosing lactose-free options can often facilitate smoother digestion. Additionally, incorporating healthy fats like avocado in moderation can provide essential nutrients. Smoothies can be a useful dietary tool; they allow for combining multiple food groups while making them easier to digest. When preparing smoothies, include fruits and vegetables that are lower in fiber and easy on the stomach, such as spinach and peaches. It’s also recommended to avoid carbonated beverages, as they can cause bloating and exacerbate symptoms. A well-rounded approach to nutrition can help patients feel better and maintain their health long-term. The goal is to nourish the body while respecting its limits. Individual approaches may vary, and what works best is oftentimes learned through trial and observation.
Meal Timing and Preparation
Meal timing is another critical factor in managing gastroparesis effectively. Patients are often advised to eat smaller meals throughout the day instead of three large ones. Spacing meals every 2-3 hours can relieve pressure on the digestive system, allowing food to be processed more easily. It can be beneficial to have lighter meals in the evening to reduce any discomfort during night-time. Planning meals ahead of time ensures that the diet remains consistent, helping to avoid triggers. Foods should be prepared in a manner that minimizes effort for digestion; therefore, steaming, pureeing, or blending can be effective methods. Cooking foods until they are soft ensures they can be digested more easily. Moreover, particular attention should be given to food temperature; some individuals may find cold or room-temperature meals easier to manage. Monitoring the body’s response to specific food types and preparation can lead to better management strategies over time. Maintaining a consistent eating schedule promotes regularity and may improve symptoms significantly, highlighting the importance of mindful dietary patterns.
Hydration is crucial in the management of gastroparesis; staying well-hydrated can help alleviate some symptoms. It is recommended to drink fluids throughout the day, focusing on clear liquids that are less likely to cause stomach upset. Clear broths, herbal teas, and natural fruit juices can provide hydration and nutrients. However, one should avoid sugary drinks as they can aggravate symptoms. Creating a stable hydration routine can be beneficial for overall health; aim for around 8 cups of fluids daily, adjusting as needed according to individual tolerance. It may also be helpful to drink fluids between meals rather than during meals to prevent unnecessary fullness. If solid food intake is limited, nutrient-dense beverages can aid in meeting nutritional needs. Smoothies and meal replacement drinks may offer balanced nutrition while easing the digestive burden. It’s important to listen to the body’s cues and adapt fluid intake according to symptoms experienced. Regular monitoring of hydration levels is essential to avoid complications, showing how integral fluid balance is in managing gastroparesis effectively.
Identifying Trigger Foods
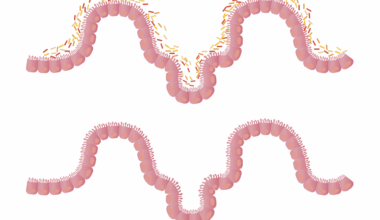
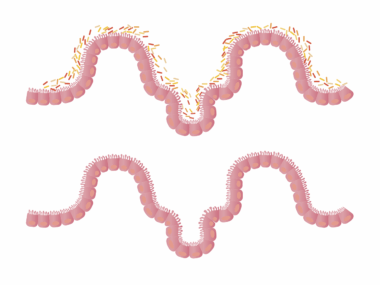
Identifying and eliminating trigger foods can significantly impact symptom management in gastroparesis. Maintaining a food diary where patients can record meals along with any related symptoms helps pinpoint problematic foods. Common triggers include high-fat meals, ground meats, nuts, and raw vegetables. Fat slows down the digestive process, while high-fiber foods can create additional work for the stomach. Instead, patients should focus on easily digestible foods with acceptable alternatives. For instance, instead of raw veggies, cooked or pureed versions are advised. Eliminating trigger foods often results in symptom improvement, leading to better overall well-being. Collaborating with healthcare providers or dietitians enhances this process by ensuring nutritional adequacy. Gradual food reintroduction after an elimination phase can clarify tolerability. By staying informed and adaptive, patients can craft a personal eating plan that reduces discomfort. Understanding food labels is also vital; ingredients can often determine how well tolerated a food item is. Each individual might have specific reactions, so personal vigilance plays an important role in the dietary management of gastroparesis.
While dietary management is vital for those living with gastroparesis, wellness goes beyond food choices. Incorporating a routine that includes gentle exercise and mindfulness practices can complement dietary efforts. Low-impact exercises, such as walking or yoga, can enhance digestive motility and overall well-being. Engaging in these activities regularly can alleviate stress, which often complicates symptoms. Stress management techniques like meditation and deep-breathing exercises can also provide substantial benefits. Connecting with a support group, either in-person or online, adds an extra layer of emotional support. Sharing experiences and strategies with others who understand can foster resilience. Creating a balanced lifestyle with several wellness dimensions can provide a sense of control and empowerment. Each positive change adds utility to the dietary strategies employed. It’s essential to recognize that managing gastroparesis is a journey that requires patience and flexibility. Support from family, friends, and healthcare professionals can serve as a beacon of guidance along the way. Understanding and exploring diverse wellness methods may lead to a more fulfilling life despite the challenges posed by gastroparesis.
Consultation with Professionals
Consulting healthcare professionals when managing gastroparesis is highly recommended for tailored approaches. A registered dietitian can provide important insights, individualized meal planning, and help navigate food intolerances effectively. They can help ensure that patients meet their nutritional needs while staying compliant with dietary restrictions. Furthermore, physicians may perform tests to evaluate the severity of gastroparesis and provide medications that might support gastric emptying. Such consultations will lead to an optimized management strategy; it’s not just about food but also understanding the condition holistically. Regular follow-ups help to assess the effectiveness of dietary adjustments and treatments. Keeping an open line of communication with healthcare providers encourages patients to voice concerns, ask questions, and discuss any new symptoms. With many variations of gastroparesis, it’s essential to seek professional guidance that recognizes individual circumstances. Patients may also benefit from learning about other treatment options, including medications or procedures that might alleviate symptoms. Staying proactive and partnering closely with professionals ultimately enhances the management of gastroparesis and improves the quality of life.
In conclusion, effectively managing gastroparesis through dietary strategies requires careful consideration of food choices, meal timing, hydration, and lifestyle modifications. It’s a multidimensional approach that emphasizes the importance of personalized nutrition. Individuals are encouraged to work collaboratively with healthcare providers to navigate their unique challenges successfully. Achieving a balance of enjoyment and healthfulness in the diet is essential; this ensures one maintains a positive attitude toward eating. Monitoring the body’s responses to various foods and adjusting cooking methods can build confidence in personal dietary management. The dynamic aspect of a gastroparesis diet encourages individuals to experiment, maintaining flexibility and openness. By being mindful of personal triggers and staying hydrated, patients can improve their symptoms considerably. Above all, the support system plays a crucial role in fostering motivation and resilience. Finally, remember that living with gastroparesis is an ongoing journey. The insights gained from experience help create a sustainable dietary lifestyle, allowing those affected to thrive despite their condition.