The Connection Between Gut Disorders and Autoimmune Diseases
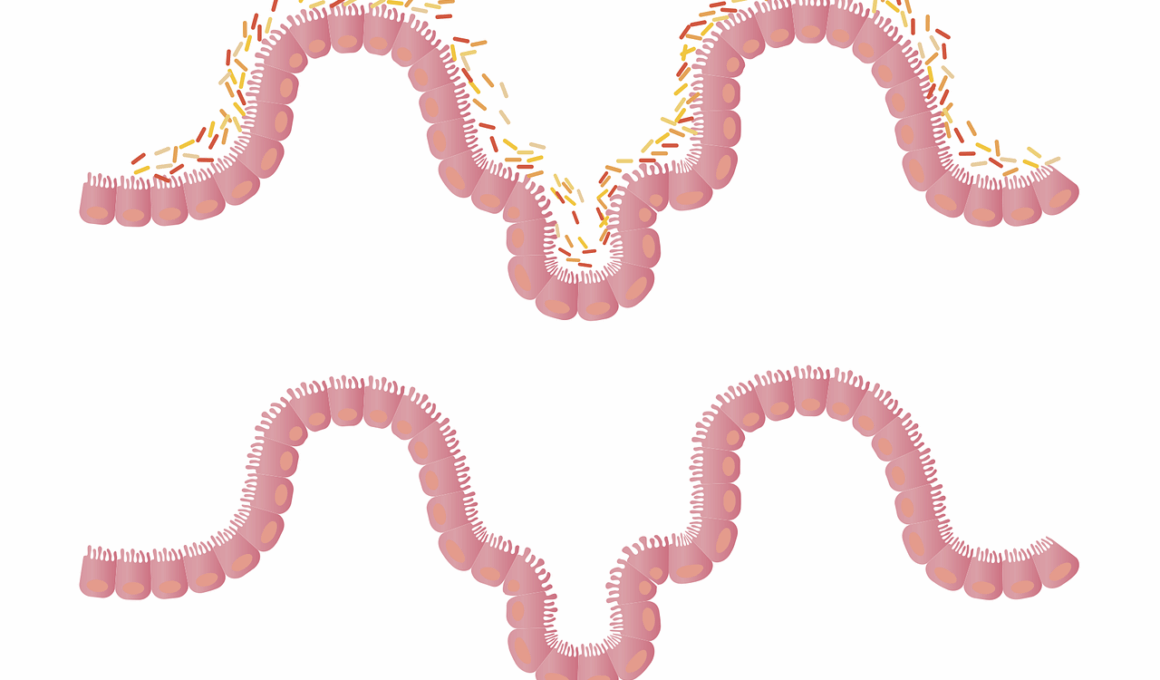
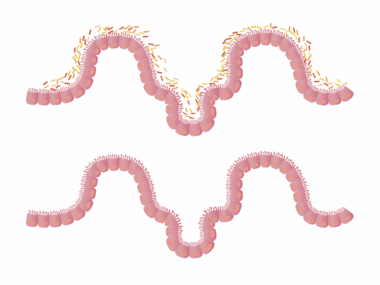
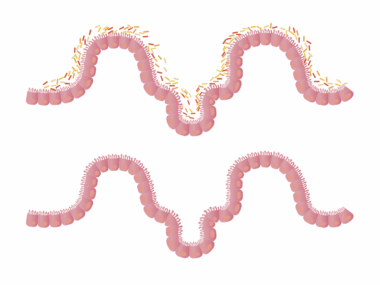
Gut health plays a critical role in overall wellness, impacting various bodily systems, including the immune system. The gut microbiome, a complex community of microorganisms, influences inflammation and immune responses. Disruptions in gut bacteria can lead to dysbiosis, which is linked to autoimmune diseases like rheumatoid arthritis and lupus. Autoimmunity occurs when the body mistakenly attacks its tissues, and research shows that an impaired gut barrier may allow toxins to enter the bloodstream, triggering inflammation. The interplay between gut health and autoimmunity highlights the importance of maintaining a balanced microbiome. Diet, lifestyle, and stress management all contribute to gut health. Probiotics and prebiotics can support beneficial bacteria, promoting gut stability. Furthermore, fermented foods like yogurt and kefir provide necessary nutrients for a healthy gut. On the other hand, a diet high in processed foods can adversely affect gut health. Monitoring gut health could help in preventing autoimmune conditions. Researchers are actively studying how gut health influences autoimmune pathology, aiming to identify potential treatments through microbiome modulation. Understanding these connections is essential for holistic health strategies and effective disease management.
Common Gut Disorders Linked to Autoimmunity
Several common gut disorders are associated with autoimmune diseases, with conditions like irritable bowel syndrome (IBS) and inflammatory bowel disease (IBD) gaining attention. IBS affects millions and often involves symptoms like bloating, gas, and abdominal pain. It can significantly impact daily life, leading to decreased quality of life. On the other hand, IBD, which includes Crohn’s disease and ulcerative colitis, represents a more severe chronic inflammatory condition that can lead to significant complications. Research indicates a strong link between these gut disorders and autoimmune diseases. Individuals with IBD have a higher risk of autoimmune disorders due to the resulting inflammation and dysregulation of the immune system. Diagnostics typically involves endoscopy, imaging, and biopsies, yet many patients remain undiagnosed for extended periods. A multidisciplinary approach involving gastroenterologists, dietitians, and immunologists is crucial for managing these conditions effectively. The common thread is the inflammatory responses in the gut leading to systemic complications. This necessitates a deeper understanding of the gut-immune axis to explore new treatments and intervention strategies.
Autoimmune diseases affect nearly 24 million people in the United States, many of whom also suffer from gut disorders.
The Role of Diet in Gut Health
Diet plays a pivotal role in maintaining gut health and potentially mitigating autoimmune disorders. A well-balanced diet rich in antioxidants, fiber, and healthy fats promotes microbiome diversity. Foods such as fruits, vegetables, whole grains, and lean proteins nourish gut bacteria, enhancing their beneficial effects. On the contrary, diets high in sugar, unhealthy fats, and artificial additives can disrupt microbial balance, exacerbating gut issues and inflammation. Research suggests that dietary interventions can alleviate the symptoms of autoimmune diseases by supporting gut flora. Strategies like the elimination diet, where potential allergens are removed temporarily, can reveal food intolerances affecting gut health. Moreover, incorporating omega-3 fatty acids from fish or flaxseeds can reduce inflammation and improve immune function. Personalized nutrition plans tailored to individual gut health status are increasingly prescribed by healthcare professionals. This emphasizes the significant impact of dietary choices on gut health, thereby influencing autoimmune disease progression. Furthermore, staying hydrated and practicing mindful eating can also positively alter gut microbiota composition, fostering better health overall.
The human gut contains trillions of microorganisms that play essential roles in our bodies.
Impact of Stress on Gut Disorders
Stress influences gut health significantly, triggering or exacerbating various gut disorders while impacting autoimmune conditions. Psychological stress can lead to changes in gut permeability, often referred to as ‘leaky gut.’ This condition allows larger particles to enter the bloodstream, potentially activating immune responses and initiating autoimmune attacks. Stress also alters gastrointestinal motility, which can lead to symptoms of IBS and IBD, thus worsening the existing gut health issues. Stress management techniques such as mindfulness, yoga, and cognitive behavioral therapy have shown positive effects on gut health and autoimmune diseases. Studies indicate that individuals who manage stress effectively report fewer symptoms related to their gut disorders. Creating a supportive environment and building resilience through these techniques can promote gut health and reduce disease severity. Furthermore, regular physical activity is known to alleviate stress and improve gut microbiota diversity. Prioritizing mental health complements physical health, creating a holistic approach to treating autoimmune diseases. By addressing both mind and body, patients may experience better outcomes in managing their gut-related ailments and overall health.
An individual’s gut microbiome can also shift according to various lifestyle factors and environmental exposures.
Future Directions in Research
Understanding the link between gut disorders and autoimmune diseases is an evolving area of scientific research. Current studies are focusing on further delineating how the gut microbiome impacts immune function. Researchers are exploring whether modulating the gut microbiota through probiotics or fecal microbiota transplantation could serve as potential therapies for autoimmune diseases. Clinical trials are essential to ascertain efficacy and safety. Additionally, examining the connection between specific strains of gut bacteria and autoimmune responses could offer new diagnostic criteria or treatment targets. Advances in genomic and metabolomic technologies are paving the way for personalized medicine approaches. The identification of unique microbiome signatures associated with autoimmune patients could lead to bespoke interventions. Furthermore, there is growing interest in understanding how lifestyle factors such as sleep, hydration, and exercise also modify gut microbiota. Collaborative efforts among immunologists, dietitians, and gastroenterologists are necessary to generate comprehensive treatment plans. Future research will undoubtedly shed light on this intricate connection, transforming how healthcare providers approach both gut health and autoimmune disease management.