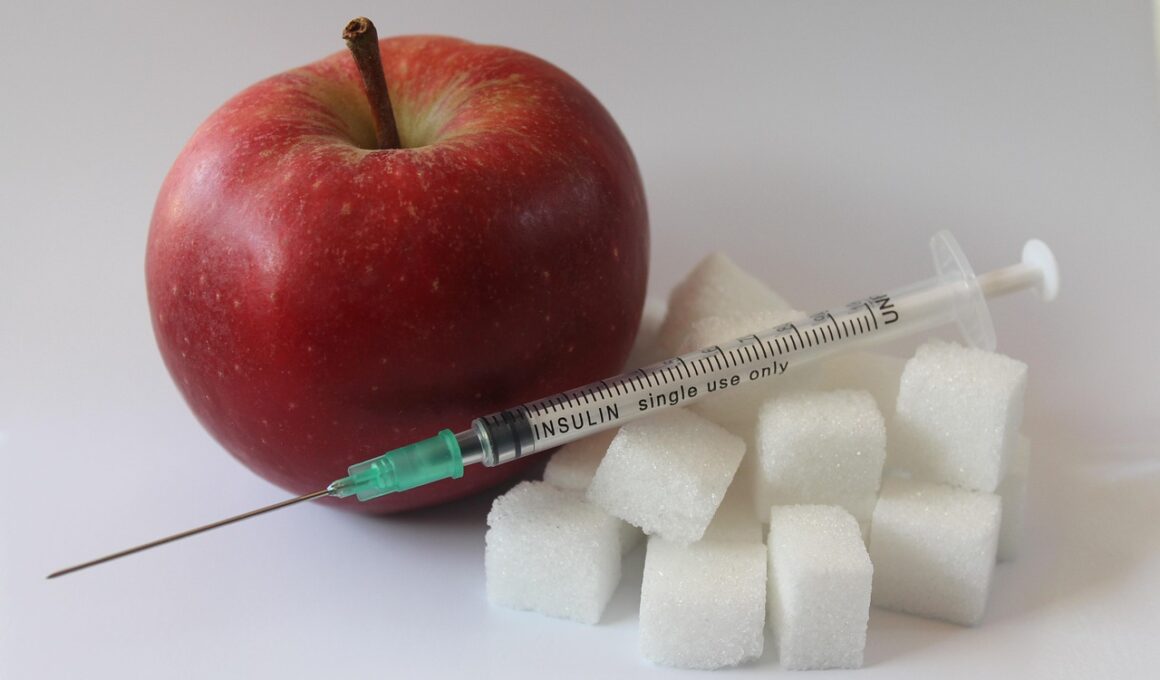
Fasting and Inflammation Reduction in Diabetes
Fasting has gained attention for its potential benefits in diabetes management, particularly in reducing inflammation. In diabetes, chronic inflammation can exacerbate insulin resistance and contribute to complications. Research shows that fasting can promote beneficial changes in inflammatory markers, which can be crucial for diabetes patients. Intermittent fasting and prolonged fasting both have positive effects on metabolic health and inflammation levels. When the body undergoes fasting, it shifts to a state of autophagy, which helps remove damaged cells contributing to inflammation. Studies suggest that fasting may lower levels of pro-inflammatory cytokines, such as TNF-alpha. Furthermore, it increases the production of anti-inflammatory molecules, enhancing overall health. In addition to the biochemical effects, fasting can influence lifestyle choices leading to healthier eating patterns. This can result in long-term benefits in weight management and homeostasis of blood sugar levels. This interplay between fasting and inflammation presents a compelling case for integrating fasting into diabetes treatment plans. Overall, understanding fasting’s role in inflammation could lead to better health outcomes for those with diabetes.
Fasting is also linked to improved insulin sensitivity, which plays a significant role in diabetes management. Insulin sensitivity refers to how effectively cells respond to insulin, the hormone that allows sugar to enter cells. In many individuals with type 2 diabetes, insulin sensitivity is compromised, leading to elevated blood sugar levels. By incorporating fasting, individuals can experience a reduction in insulin resistance, allowing better glucose regulation. Observational studies indicate that individuals practicing intermittent fasting experience significant reductions in fasting insulin levels. This might lead to improved blood sugar control over time, essential for diabetes patients. Moreover, fasting can help reduce body weight, a critical factor in managing diabetes. Weight loss is associated with improved insulin sensitivity and reduced inflammation, both contributing to better overall health. Incorporating fasting routines can also encourage mindful eating practices. Traditional dietary guidelines often emphasize the importance of nutrient-dense choices; however, fasting can provide a structured approach to eating that facilitates these habits. The long-term benefits of improved insulin sensitivity from fasting can play a vital role in diabetes prevention and management.
Fasting and Reduced Oxidative Stress
An essential aspect of inflammation in diabetes is oxidative stress, which occurs when free radicals surpass the body’s defensive capabilities. Oxidative stress contributes significantly to chronic inflammation and subsequent complications associated with diabetes. Fasting has demonstrated potential in decreasing oxidative stress levels, which may also be linked to inflammation reduction. Various studies show that fasting can enhance the body’s antioxidant defenses. By doing so, it may help protect against the cellular damage typically seen in diabetes. Antioxidants can neutralize free radicals, thereby reducing inflammation and promoting better overall health. Additionally, during fasting, the body undergoes metabolic adaptations that further contribute to decreased oxidative stress. These adaptations may also improve cellular function and stability in insulin-sensitive tissues. As more individuals adopt intermittent fasting as a lifestyle choice, monitoring its impacts on oxidative stress and inflammation is essential. This also opens the door for utilizing fasting as a complementary approach in treating various diabetes-related complications and general well-being. Improved oxidative balance can result from a single fasting regimen, underscoring the potential power of fasting in diabetes management.
Aside from metabolic changes, the mental health benefits of fasting are also noteworthy. Diabetes management can be a psychological burden, given the constant need to monitor blood glucose levels and the associated dietary restrictions. Fasting may offer a mental reset, allowing individuals to gain control over their eating habits and alleviate anxiety related to food choices. Furthermore, fasting encourages a simplified approach to eating, which might support better mental clarity and concentration. Some studies suggest that fasting can promote neuroprotective effects due to decreases in inflammation, positively impacting cognitive function. Mindful fasting practices can foster a healthier relationship with food and encourage self-discipline. It serves as an opportunity to reinforce goals around health and well-being, fostering an empowered mindset towards diabetes management. Alongside these psychological benefits, the increased sense of community among those practicing fasting can create meaningful social support networks. Connecting with others who are also managing diabetes through fasting can greatly enhance motivation and accountability. Consequently, the psychological benefits of fasting can have a ripple effect on how individuals handle diabetes in daily life.
Practical Tips for Implementing Fasting
For individuals considering fasting as a strategy for managing diabetes, several practical tips can assist in implementing this approach safely and effectively. First, it’s recommended to consult healthcare professionals before starting any fasting regimen, especially for those on medications affecting blood sugar. Gradually introducing intermittent fasting can ease the transition, starting with just a few hours, and then progressively increasing fasting periods. This method helps the body adapt while reducing the risk of ketone production for those on insulin. Choosing nutrient-dense foods during eating windows is vital; prioritizing whole grains, vegetables, and proteins can stabilize blood sugar levels. Staying hydrated during fasting is equally important, promoting optimal body function and reducing hunger pangs. Incorporating regular physical activity can further enhance the benefits of fasting, promoting cardiovascular health and aiding in weight management. Additionally, tracking blood sugar levels consistently during fasting will provide insights into how the body responds, ensuring safety. Lastly, remaining flexible in fasting plans allows individuals to adjust based on personal schedules and well-being. This adaptability ensures a sustainable approach to fasting that can maintain long-term benefits.
Research continues to unveil new information regarding the connection between fasting, inflammation, and diabetes management. Recent studies are focusing specifically on different fasting approaches and their effects on inflammation markers in diabetes patients. For instance, a combination of both intermittent and alternate-day fasting might provide unique advantages over traditional caloric restriction. Understanding how these various fasting strategies influence inflammation could pave the way for personalized dietary interventions tailored for individuals with diabetes. Clinical trials are increasingly exploring the relationship between fasting routines and clinical outcomes related to inflammation markers. Gathering more evidence can significantly impact diabetes education and treatment plans. As new findings emerge, there is a promising outlook towards integrating fasting as a methodology for improving diabetes-related inflammatory conditions. A multi-disciplinary approach involving nutritionists, endocrinologists, and mental health professionals can help individuals navigate their fasting journeys safely. Community support is also integral to fostering adherence and success. Fasting could be more than just a diet; it is strengthening the notion of holistic health that empowers individuals living with diabetes.
Conclusion
In conclusion, fasting demonstrates several potential benefits for individuals managing diabetes, particularly in reducing inflammation. As inflammation plays a critical role in advancing diabetes complications, leveraging fasting could serve as a preventative strategy. Improved insulin sensitivity, reduced oxidative stress, and mental health benefits underscore the multifaceted advantages of fasting. However, it is crucial to approach fasting thoughtfully and in a manner consistent with individual health needs. For optimal results, personalized guidance from healthcare providers can help navigate the complexities associated with fasting and diabetes management. As research continues to evolve, the potential role of fasting in overall diabetic care may broaden. Individuals may find inspiration in fasting’s adaptability and accessibility, promoting healthier lifestyles. The continuous dialogue about fasting highlights the necessity for individualized approaches in dietary recommendations. This encourages a proactive attitude toward diabetes and health management. Embracing these holistic methods can empower individuals living with diabetes to take charge of their health, ultimately leading to improved quality of life and well-being. Fasting could represent a significant ally in the ongoing therapeutic journey of diabetes care.