Exploring the Role of Gut Bacteria in Bipolar Disorder
The gut microbiome is a complex ecosystem that influences various aspects of our health, including mental well-being. The connection between gut bacteria and bipolar disorder is an emerging area of study that highlights the importance of a balanced microbiome. Research indicates that individuals suffering from bipolar disorder often experience alterations in their gut microbiota. These changes can lead to inflammation, which is believed to play a significant role in mood regulation. Probiotics and prebiotics can help restore gut health and improve symptoms. Various studies suggest that the supplementation of specific probiotic strains could mitigate mood swings. Moreover, these beneficial bacteria can produce neurotransmitters like serotonin and gamma-aminobutyric acid (GABA), contributing to better mood stability. Maintaining a healthy diet rich in fiber, fruits, and vegetables can support the growth of good bacteria. Conversely, diets high in processed foods may exacerbate symptoms. Future research is vital in establishing the direct causative links between gut health and mental disorders. Understanding these connections will open avenues for potential treatments that target the gut as a pathway to improve mental health outcomes.
The Gut-Brain Connection Explained
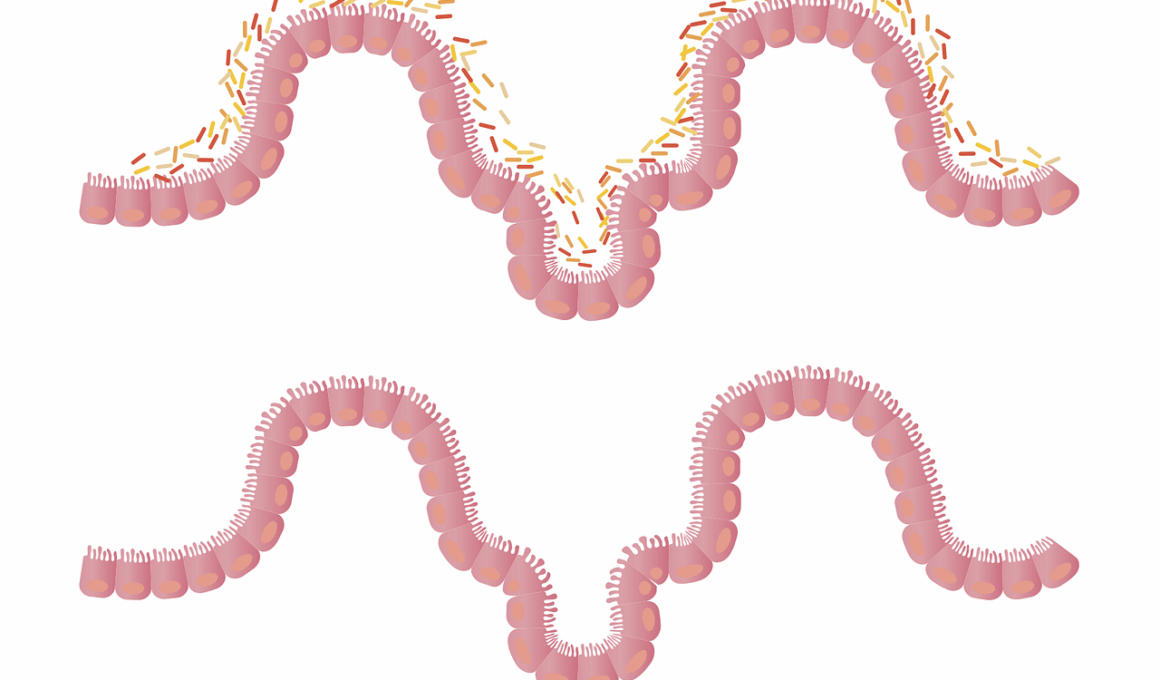
The gut-brain axis is a bidirectional communication system between the gastrointestinal tract and the brain. This physical and functional connection allows gut bacteria to influence brain function via the vagus nerve and other pathways. Significantly, this connection involves neurotransmitters, hormones, and immune mediators that signal to the brain. Researchers have found that disturbances in the gut microbiome can lead to inflammatory responses that affect brain health and mood. For instance, studies have shown that an imbalance in gut bacteria can contribute to the development of anxiety and depression, which often coexist with bipolar disorder. The microbiota interacts with the central nervous system, impacting behaviors, cognition, and emotional states. Treatments aiming to regulate gut health could potentially enhance mood stabilization in individuals with bipolar disorder. Incorporating lifestyle changes can support this process. For instance, enhancing diet, reducing stress, and increasing physical activity can positively affect gut flora. More studies are needed to fully understand this gut-brain relationship, but the potential for holistic approaches combining diet, supplementation, and mental health treatment exists. The findings represent an intriguing frontier in mental health.
Exploring specific gut bacteria associated with bipolar disorder is imperative for future treatments. Research indicates that certain bacterial strains may have protective benefits against mental health disorders. For example, Lactobacillus and Bifidobacterium species have been associated with improved mood and reduced anxiety levels. In contrast, an abundance of pathogenic bacteria can lead to inflammation and negatively affect neurotransmitter levels, exacerbating mood fluctuations. By identifying and cataloging these beneficial bacteria, researchers can develop targeted probiotic formulations specifically designed for individuals with bipolar disorder. Additionally, personalized nutrition strategies tailored to foster microbial diversity could serve as an adjunct treatment. It’s also essential to consider the role of diet in modulating gut bacteria. A diet high in omega-3 fatty acids can potentially boost beneficial microbiota while suppressing pathogenic strains. Moreover, the gut microbiome’s influence on inflammation highlights the need for an anti-inflammatory approach in dietary interventions. Introducing foods rich in antioxidants and fermentable fibers can also support a healthy microbiome. Overall, advancing our understanding of these microbial relationships will be crucial in developing comprehensive treatment plans that incorporate both diet and mental health therapies.
Potential Therapeutic Approaches
As research continues to uncover the connections between gut microbiome and bipolar disorder, various therapeutic approaches are emerging. One promising strategy involves the use of probiotics as a supplementary treatment. Probiotics are live microorganisms that confer health benefits when consumed in adequate amounts. These are believed to help balance the gut microbiome and potentially mitigate symptoms associated with bipolar disorder. Empirical studies reveal that certain probiotic strains, such as Lactobacillus rhamnosus, may aid in reducing anxiety and depressive symptoms. Another strategy includes dietary modification aimed at fostering gut health. Diets rich in whole grains, lean proteins, fruits, and vegetables can enhance the diversity of gut bacteria. Furthermore, reducing sugar and saturated fats may lessen inflammation and promote better mood regulation. Incorporating fermented foods into the diet, like yogurt, kimchi, and kombucha, can further enrich beneficial microbial populations. Additionally, lifestyle interventions emphasizing stress management, regular exercise, and adequate sleep contribute significantly to gut health and, ultimately, mood stabilization. These potential therapeutic approaches represent a multidimensional strategy to tackle bipolar disorder more holistically, focusing not just on the brain but also on gut health.
Despite the potential benefits of targeting gut health in bipolar disorder treatment, challenges and limitations persist. The field is still in its infancy, and much of the existing research relies on animal study data rather than clinical trials involving humans. This may hinder the translation of findings into actual treatments. Additionally, individual variability in gut microbiota complicates the establishment of one-size-fits-all interventions. Factors such as genetics, lifestyle, and pre-existing medical conditions can influence how the microbiome responds to dietary or probiotic interventions. Standardized measures to assess gut health and mental well-being are also lacking. Moreover, more extensive and well-designed studies are necessary to clarify causative relationships. It’s essential to ensure that microbial treatments do not unintentionally cause adverse reactions or exacerbate existing conditions. Collaboration between microbiologists, mental health professionals, and dietitians is crucial in developing comprehensive care strategies. The future looks promising, but caution and methodological rigor will be necessary to navigate the complex interactions between gut bacteria and mental health. Addressing these challenges squarely will lead to tangible changes in how we approach treating bipolar disorder focuses on holistic health.
Conclusion and Future Directions
In conclusion, the link between gut microbiota and bipolar disorder represents a fascinating intersection of nutrition and mental health. As our understanding of the microbiome deepens, the potential for innovative treatment options remains bright. Future research is critical for uncovering effective probiotics and dietary approaches tailored to improve psychiatric health. Investing in multidisciplinary research efforts will pave the way for breakthroughs that extend beyond bipolar disorder to encompass broader psychiatric conditions influenced by gut health. It will also be critical to emphasize prevention measures, including dietary education and lifestyle adjustments that promote gut health as a proactive approach. Initiatives aimed at increasing public awareness of the gut-brain connection could empower individuals to make informed lifestyle choices that benefit both their mental and physical health. The importance of an interdisciplinary approach cannot be underestimated. By synthesizing insights from psychology, nutrition, and microbiology, we can form a comprehensive treatment paradigm that not only addresses bipolar disorder but also enhances overall mental well-being. As emerging research continues to shed light on this connection, we may soon see a paradigm shift in how we understand and treat mental health disorders.
Ultimately, further studies exploring how specific dietary patterns influence the gut microbiome in individuals with bipolar disorder will be essential. This research could contribute to a more profound understanding of how targeting gut health can ameliorate mood regulation. The dynamic relationship between diet, gut bacteria, inflammation, and mood represents an exciting frontier in scientific inquiry. As our knowledge expands, healthcare practitioners may integrate microbiome-focused strategies into their practice, resulting in more tailored and effective treatments. Encouraging a holistic approach to mental health that emphasizes gut health could redefine traditional paradigms. Engaging in personalizing treatments based on one’s microbiome composition has tremendous potential, suggesting we are on the brink of a healthcare revolution. Fostering collaboration among various fields will allow researchers and clinicians to explore the far-reaching implications of gut health on mental well-being deeply. As research progresses, the integration of gut health and mental health could transform how we approach treatment and prevention, ultimately leading to improved outcomes for individuals living with bipolar disorder and other mental health conditions.
The Future of Gut Microbiome Research
The future of research on gut microbiomes is budding with new possibilities and revelations in mental health treatment. As we gather more data about the specific microbial compositions impacting disorders like bipolar disorder, potential prevention and therapeutic techniques become clearer. This might lead to individualized treatments based on gut microbial profiles, allowing for tailored dietary and probiotic interventions. Furthermore, continued advancements in genomic technologies will play a critical role in understanding microbial interactions at play in mental health disorders. Studies examining the longitudinal effects of diet on gut microbiota will yield valuable insights into preventive measures. Promoting healthy eating habits to individuals at risk may prove beneficial in mitigating the severity of symptoms associated with bipolar disorder. Moreover, initiatives aimed at enhancing the public’s understanding of the gut-brain axis will encourage proactive health management. Research on this intersection also underscores the importance of early intervention and continuous management strategies. Combining modern medicine with practical lifestyle advice can change the landscape of mental health care. As the field evolves, interdisciplinary collaboration will remain essential to advancing our understanding of mental health through the lens of gut microbiome research.