Stress-Related Changes in the Gut Microbiome
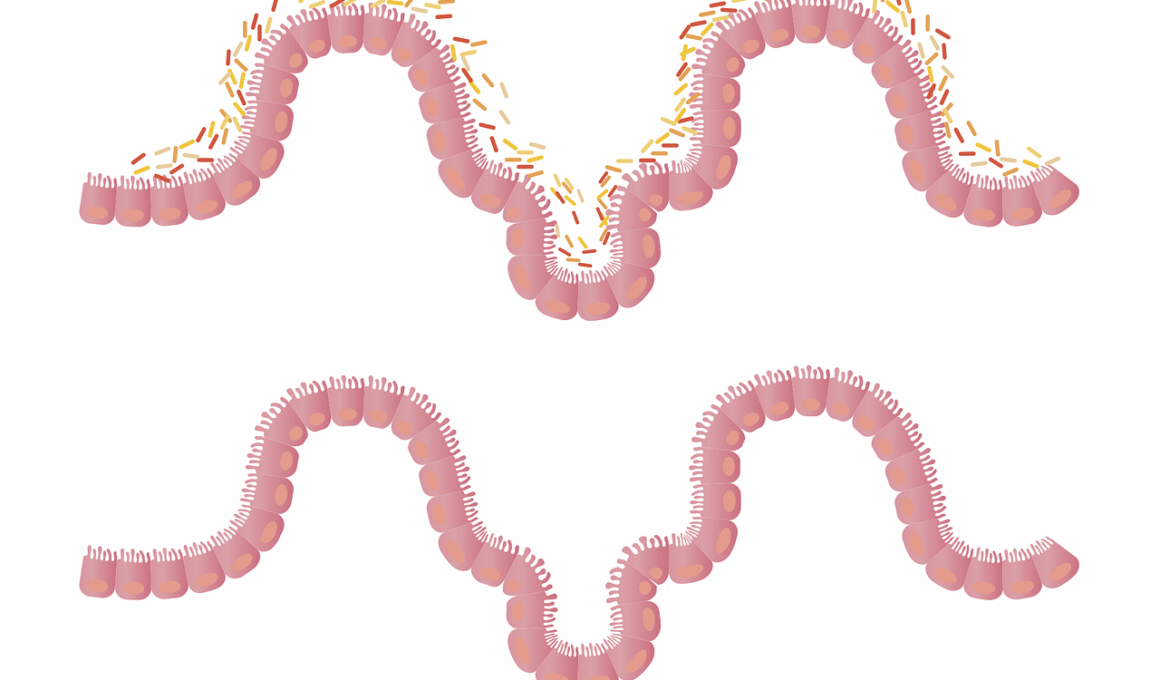
Chronic stress significantly influences the gut microbiome, leading to various gastrointestinal disorders. The gut microbiome comprises trillions of microorganisms that contribute to digestion, metabolism, and immune function. Stress can alter this delicate balance, resulting in an overgrowth of harmful bacteria while reducing beneficial bacteria. These changes can manifest as digestive issues, such as irritable bowel syndrome (IBS), inflammatory bowel disease (IBD), and dysbiosis. Furthermore, chronic stress triggers the release of stress hormones like cortisol, which exacerbate these imbalances. Studies suggest that stress-induced changes in the gut microbiome can affect the gut-brain axis, a bidirectional communication pathway linking the gut and brain. This interaction may provoke anxiety and depression, creating a cycle of stress and gastrointestinal dysfunction. Maintaining a healthy gut microbiome through stress management techniques is crucial in preventing these disorders. Approaches such as yoga, meditation, and mindfulness have shown promise in improving gut health. Therefore, understanding the impact of chronic stress on gut health can lead to effective interventions and enhance overall well-being. Further research is needed to explore this complex relationship in greater detail.
One crucial aspect of managing stress-related gastrointestinal disorders is dietary modifications. The gut microbiome thrives on a diverse diet rich in fiber, vitamins, and minerals. Foods such as fruits, vegetables, whole grains, and fermented products promote the growth of beneficial bacteria. Conversely, diets high in sugar and saturated fats can negatively affect this balance. Research indicates that specific probiotics may alleviate symptoms associated with gut dysbiosis related to stress. Probiotics contain live beneficial bacteria that contribute positively to gut health. Incorporating these into daily nutrition can help restore balance in the microbiome and mitigate stress’s impact on digestion. Following a balanced and nutritious diet, coupled with proactive stress management strategies, offers promising avenues for improvement. Staying hydrated is equally essential, as dehydration can lead to digestive issues. As chronic stress persists, it’s important to address both psychological factors and lifestyle habits. Stressful situations often result in poor eating choices, further affecting gut health. Ultimately, a comprehensive approach integrating nutrition and stress management is essential for fostering a balanced gut microbiome. Recognizing these connections empowers individuals to adopt healthier behaviors and improve overall health.
Gut-Brain Axis and Stress
The gut-brain axis plays a vital role in understanding how chronic stress affects gut health. This complex system involves communication between the gastrointestinal tract and the brain, influencing emotional and physical well-being. Stress can disrupt the gut’s normal functioning, leading to altered gut permeability and inflammation. Increased gut permeability, often referred to as “leaky gut,” allows harmful substances to enter the bloodstream, potentially leading to systemic inflammation. This inflammatory response can affect brain function and contribute to mental health disorders, such as anxiety and depression. Notably, the gut microbiome produces neurotransmitters, including serotonin, which regulates mood. An imbalance in gut bacteria caused by stress might lead to reduced serotonin production, further exacerbating feelings of anxiety or depression. Thus, stress-induced changes in the microbiome may create a feedback loop that perpetuates gastrointestinal symptoms and mental health issues. Recognizing the gut-brain connection highlights the importance of treatment strategies addressing stress management and gut health. Effective interventions should encompass both psychological support and nutritional guidance, fostering a balanced gut microbiome and improved emotional regulation. Understanding this significant relationship can inform therapeutic approaches to aid individuals experiencing stress-related gastrointestinal disorders.
Another important dimension of chronic stress and gastrointestinal disorders is the role of inflammation. Stress triggers the release of pro-inflammatory cytokines, which can adversely impact gut health. Chronic inflammation is linked to various gastrointestinal conditions, including IBD. A balanced gut microbiome helps regulate immune responses, minimizing inflammation. However, stress-induced dysbiosis can lead to an overactive immune response, perpetuating a state of inflammation. Managing inflammation through stress reduction and dietary changes becomes paramount in mitigating these issues. Antioxidant-rich foods, such as berries, leafy greens, and nuts, can help combat oxidative stress and inflammation. Regular physical activity also plays a role in reducing inflammation and improving gut health via positive changes in the microbiome. Engaging in stress-relief techniques like deep breathing, yoga, and progressive muscle relaxation may support the gut’s recovery process. By addressing both mental and physical health aspects, individuals can significantly impact their gut microbiome. Additionally, seeking professional help can further guide management approaches. Understanding the relationship between chronic stress, inflammation, and gut health empowers individuals to make informed choices, contributing to better health outcomes in the long run.
The Role of Lifestyle Interventions
Lifestyle interventions can effectively address chronic stress and its impact on gastrointestinal disorders. Emphasizing stress management techniques is crucial for promoting gut health. Effective strategies include regular exercise, balanced nutrition, and adequate sleep. Exercise has proven benefits for both stress relief and gut health. Activities such as walking, jogging, or yoga can enhance mood and reduce stress hormones, thereby fostering a healthier gut microbiome. Nutrition is equally important; a well-balanced diet is essential to support physiological health. Consuming a variety of whole foods, such as fruits, vegetables, and legumes can enrich the gut microbiome and mitigate stress effects. Additionally, prioritizing sleep can significantly impact stress levels and gut function. Insufficient sleep disrupts hormone levels and can exacerbate digestive issues. Establishing a consistent sleep routine and creating a restful environment are vital components of overall health. Furthermore, social support and mindfulness practices can reinforce lifestyle changes. Connecting with friends and family reduces stress and improves emotional well-being. Thus, employing a multifaceted approach integrating these lifestyle interventions can positively influence gut health while managing chronic stress effectively.
The scientific community continues to explore the intricate relationship between chronic stress and gut disorders. Emerging research highlights the potential of the gut microbiome as a target for therapeutic interventions. This area of study has led to the increased interest in probiotics and prebiotics for managing stress-related gastrointestinal issues. Probiotics are live microbes that confer health benefits when consumed in adequate amounts, while prebiotics serve as food for beneficial gut bacteria. Regular consumption of these substances may promote a healthier gut microbiome, positively influencing mood and stress resilience. Moreover, personalized approaches based on individual microbiome profiles could enhance treatment outcomes. Genetic, lifestyle, and environmental factors shape the unique composition of each person’s microbiome. Identifying specific strains of probiotics that suit individual needs presents new avenues for treatment. The shift towards a more personalized medicine approach enables clinicians to tailor interventions better. With ongoing research, our understanding of the gut microbiome’s involvement in stress and gastrointestinal health will deepen, leading to innovative and effective treatment options. Thus, the future of managing stress-related gastrointestinal disorders looks promising, offering hope for those affected.
Conclusion: A Holistic Approach
In conclusion, addressing chronic stress and its effects on gut health requires a comprehensive and holistic approach. Recognizing the interconnectedness between stress, the gut microbiome, and gastrointestinal disorders is essential for effective management. Incorporating dietary modifications, stress management techniques, lifestyle interventions, and personalized treatments can significantly enhance overall well-being. Individuals should be aware of the influence of stress on their gastrointestinal health and engage in proactive strategies to maintain a balanced gut microbiome. Emphasizing nutrition, regular exercise, and adequate sleep will provide the foundation for successful interventions. Collaboration between healthcare providers, nutritionists, and mental health professionals can ensure integrated care that considers both physical and mental health. Continuous research investigating the microbiome’s role in stress resilience will inform future therapeutic options. Meanwhile, understanding this relationship empowers individuals to make meaningful lifestyle changes, fostering a healthier gut and improved emotional balance. Ultimately, a holistic approach can improve the quality of life for those affected by chronic stress and gastrointestinal disorders, paving the way for brighter health outcomes in the long run.