Gut Microbiome Variations Across Different Aging Populations
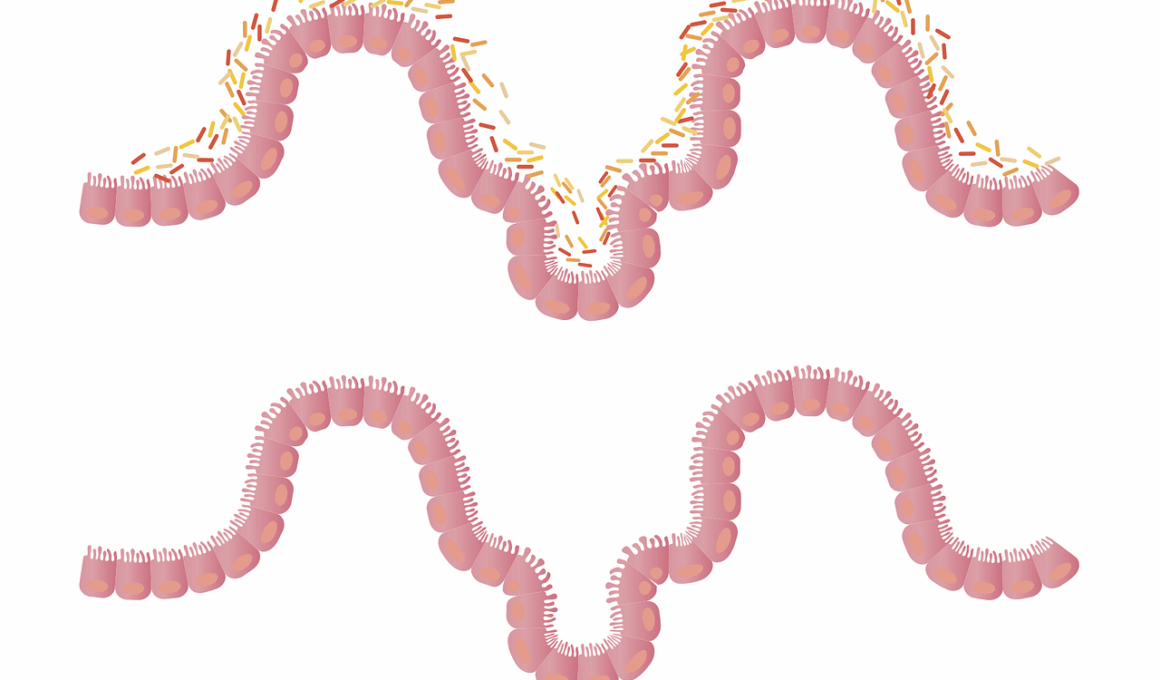
The gut microbiome undergoes significant changes as individuals age. These variations can have profound impacts on health and well-being in older populations. The composition of gut bacteria is influenced by various factors including diet, environment, and lifestyle. Older adults often experience a decrease in microbial diversity, which is linked to several health issues such as metabolic disorders and inflammation. As we age, the beneficial gut bacteria may decline, while potentially harmful bacteria may increase. This imbalance can lead to dysbiosis, a condition characterized by an unhealthy microbiome. Recent studies suggest that age-related changes in the gut microbiome influence the immune system’s functionality, resulting in a higher susceptibility to infections. Furthermore, the presence of certain bacteria has been associated with improved cognitive functions, illustrating a connection between gut health and brain health. Understanding these shifts in microbiome composition is crucial for developing targeted interventions aimed at promoting healthy aging. Maintaining a diverse gut microbiome through probiotics, dietary sources of fiber, and fermented foods can play a significant role in enhancing overall health. This approach helps mitigate the adverse effects of aging and support functional longevity.
The age-related alterations in gut microbiome are not uniform across populations. Varied geographical and cultural backgrounds influence the composition and functionality of gut bacteria. For instance, populations consuming different dietary patterns exhibit distinct microbiome profiles. Western diets, high in saturated fats and sugars, tend to promote harmful bacteria, while plant-based diets rich in fiber foster beneficial bacteria. Studies indicate that older adults from non-Western countries maintain a more diverse gut microbiome compared to their Western counterparts. This diversity is linked to a lower incidence of age-associated diseases. Moreover, older adults in rural settings often display a richer microbiome than those in urban areas, highlighting the impact of environmental factors such as exposure to nature. Understanding these disparities is essential for designing microbiome-targeted health interventions tailored to specific aging populations. Probiotic and prebiotic supplements can be customized based on the cultural dietary habits of particular communities. Researchers are exploring ways to restore healthy microbiome profiles through diet and supplementation, focusing on diversity as a key indicator of gut health. Ultimately, these findings underscore the importance of considering individual lifestyle factors when addressing gut microbiome health in aging.
Another critical aspect of understanding gut microbiome changes with aging is the influence of medications. Many older adults are prescribed multiple medications, known as polypharmacy, which can adversely affect the gut microbiome. Antibiotics, for example, can drastically reduce microbial diversity, leading to a higher risk of gastrointestinal disorders. Chronic medication use has been shown to alter the balance of beneficial and pathogenic bacteria, often resulting in dysbiosis. Research indicates that those on long-term medication regimens may experience increased inflammation and a compromised immune response. It is essential for healthcare providers to consider the potential impact of medications on gut health as they age. Monitoring gut microbiome composition in older patients can help tailor treatments that minimize negative impacts. Additionally, alternative therapies may be explored to reduce reliance on medications that disrupt gut bacteria. Encouraging appropriate dietary changes and promoting the use of probiotics may mitigate some of the adverse effects associated with medication use. This holistic approach to health care, which prioritizes gut microbiome health, is critical for enhancing life quality in aging populations. By understanding these interactions, practitioners can make informed decisions.
Impact of Chronic Diseases
The relationship between chronic diseases and gut microbiome changes is another vital area of research. Conditions such as obesity, diabetes, and cardiovascular diseases are prevalent among aging populations and have been linked to distinct gut microbiome profiles. Dysbiosis plays a crucial role in the development and progression of these diseases, with specific bacterial taxa associated with inflammation and metabolic dysregulation. For example, certain bacteria are known to influence lipid metabolism, impacting weight and glucose levels in older adults. Interventions aiming to restore a healthy microbiome could provide significant benefits for managing chronic illnesses. Lifestyle modifications, including diet, exercise, and the incorporation of probiotics, can lead to improvements in gut health, which in turn may alleviate chronic disease symptoms. Researchers are now exploring how gut microbiome manipulations can be employed alongside traditional treatment methods to enhance overall treatment effectiveness. The potential for using gut health as a therapeutic target is an exciting frontier in geriatric medicine. Understanding the interconnections between aging, chronic diseases, and gut health opens pathways for innovative approaches to health care in older populations.
Moreover, the role of diet in shaping gut microbiome changes cannot be overstated, particularly in aging populations. Consuming a diverse range of foods—particularly fruits, vegetables, whole grains, and fermented foods—can significantly enhance gut microbiome diversity. Older adults often face dietary limitations; thus, promoting accessible sources of prebiotics and probiotics within their diets is imperative. Research indicates that increasing fiber intake can positively alter gut flora, supporting the growth of beneficial bacteria. Encouraging older adults to participate in cooking and meal preparation can help foster better dietary habits, ensuring they consume a balanced diet vital for gut health. Meals that incorporate fermented foods like yogurt, kimchi, and sauerkraut are beneficial. These dietary changes can help stabilize and restore the microbial community, leading to improved health outcomes. Additionally, hydration and adequate nutrition should be prioritized during this transition. Engaging with nutritionists and dietitians to create personalized nutritional plans can be transformative. A holistic approach to nutrition that adapts to aging needs can help maintain a healthy gut microbiome, ultimately contributing to a more vibrant and healthy aging experience.
In addition to dietary interventions, the importance of physical activity in maintaining a healthy gut microbiome in aging populations should not be overlooked. Regular exercise has been shown to promote microbial diversity, partially by stimulating the growth of beneficial bacteria. Engaging in physical activity can improve gut motility and foster a more dynamic gut environment. For older adults, low-impact activities such as walking, swimming, or gardening can enhance overall physical well-being while positively influencing gut health. Effective exercise regimens foster coordination and balance, reducing the risk of falls and promoting independence. Additionally, community-based exercise programs can also offer social support, which is critical for maintaining mental health. Encouraging older adults to stay active, even with simple daily exercises, can help preserve their gut microbiome integrity. Personal trainers and physical therapists can coach older individuals on appropriate exercise routines, ensuring safety and effectiveness. A multifaceted approach that combines diet, exercise, and social engagement may demonstrate significant benefits in promoting a healthy gut microbiome in older populations. Encouraging adherence to these lifestyle changes is essential for achieving lasting health benefits.
Conclusion: The Future of Gut Microbiome Research in Aging
As we deepen our understanding of the gut microbiome’s role in aging, the implications for future health care are profound. Ongoing research holds promise for identifying microbiome-based therapies tailored to mitigate age-related conditions and enhance quality of life. The imbalance of gut microbiota is increasingly recognized as a crucial factor in various diseases, highlighting the need for further investigation. Personalized approaches, integrating nutritional, physical, and psychological factors, can lead to comprehensive strategies for health management in older populations. Developing standardized guidelines focusing on gut health for aging adults will be essential for future public health initiatives. Collaboration across various fields, including microbiology, gerontology, and nutrition, can drive innovation in the treatment and prevention of age-related conditions rooted in the microbiome. Supporting health professionals with the latest research findings will empower them to recommend appropriate interventions. As our knowledge expands, we may identify predictive biomarkers associated with gut health, allowing for proactive management of health during aging. The evolution of microbiome research holds exciting potential for transformative strategies that promote healthy aging and well-being in diverse populations.
In light of these developments, public awareness campaigns targeting gut health in aging populations will be crucial. Educating older adults and their caregivers about the importance of nutrition, exercise, and their interconnected impacts on gut microbiome can encourage proactive health decisions. Local communities should promote programs dedicated to gut health, offering resources on nutrition, exercise, and access to probiotics. Additionally, creating partnerships with health care providers will facilitate broader discussions on gut health’s role in aging. Incorporating educational workshops or seminars focused on gut microbiome research can inspire positive lifestyle choices. Technological advancements can also play a role, with mobile apps providing personalized dietary recommendations and exercise plans designed for targeted interventions. Utilizing social media platforms to spread awareness and share success stories will keep engagement high. As awareness of the gut microbiome grows, older populations can benefit from the knowledge and tools necessary to improve their gut health. Overall, a combined effort of educational initiatives, health care collaboration, and community engagement can generate positive change. Ultimately, promoting gut health is pivotal to improving life quality for aging populations.